CONTENT
- HOME PAGE
- PROLOGUE AN URBAN LEGACY
- INTRODUCING THE WEST SIDE
- 19th-CENTURY CAMERA
- URBAN PHOTOGRAPHERS HINE AND KIRKLAND
- PICTORIAL CHICAGO
- CHICAGO ENLIGHTENED CITY BEAUTIFUL
- CHICAGO GROTESQUE LAWLESS STREETS
- HULL-HOUSE "OASIS" IN A SLUM
- IMMIGRANT EMIGRANT CITY
- "ALIEN" COLONIES
- "RACE" COLONIES
- GHETTO LIVING
- "CHEAP" ECONOMY
- FAMILY
- AMUSEMENTS
- PUBLIC HEALTH
- TENEMENTS
- URBAN SOCIOLOGY CHICAGO SCHOOL
- MAXWELL STREET ARCHITECTURE TOUR
- CHICAGO CITY MAPS
“PUBLIC HEALTH” AND PEASANT MEDICINE
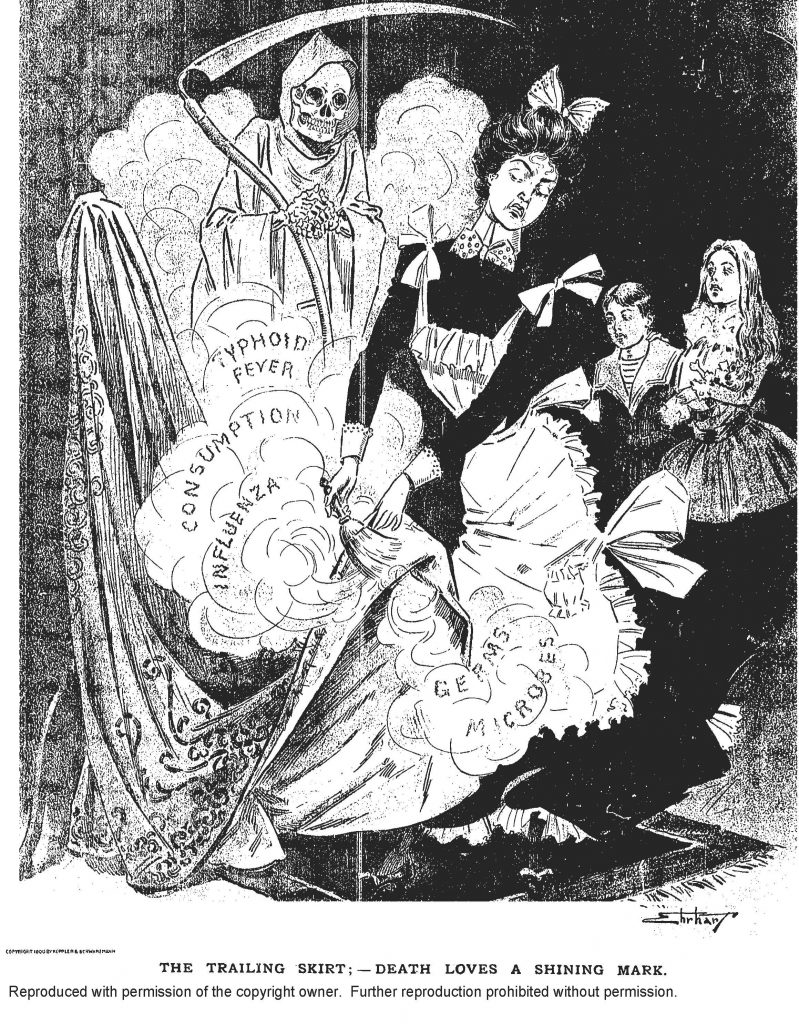
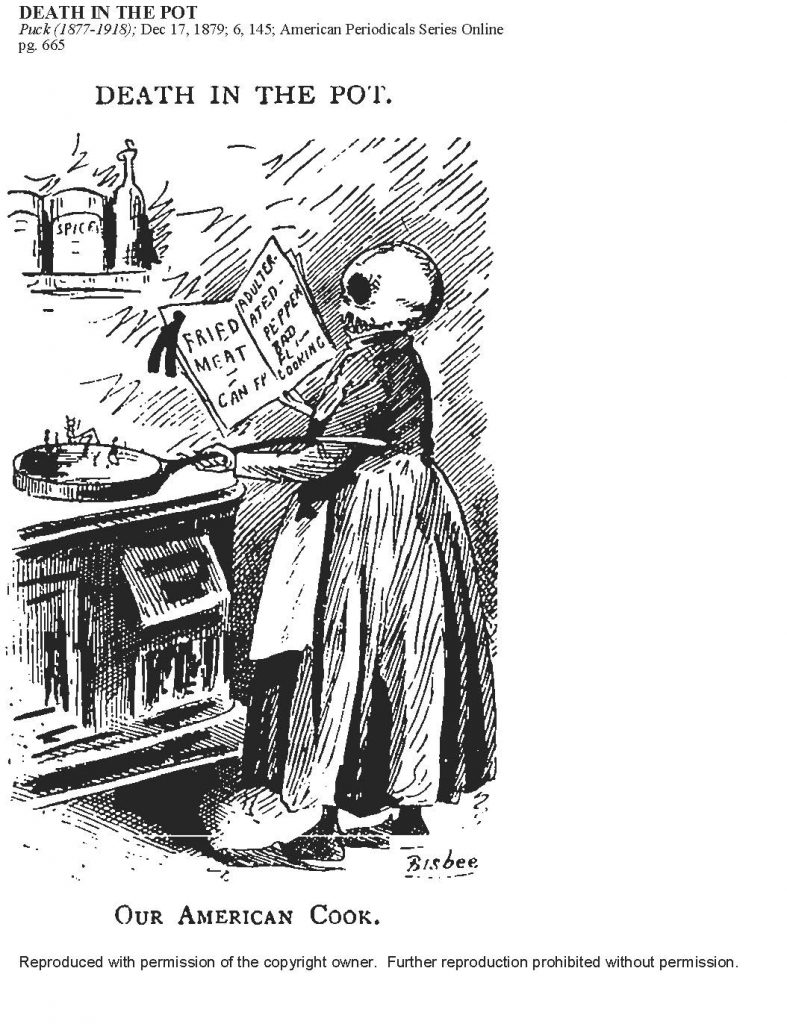
Chicago’s Near West district was densely populated by immigrant working peoples living in an industrial zone including manufacturing, shipping, railways, and markets. It was not a healthy area to live and work in with substandard housing. garbage and sewage strewn on the streets, and failing city services.
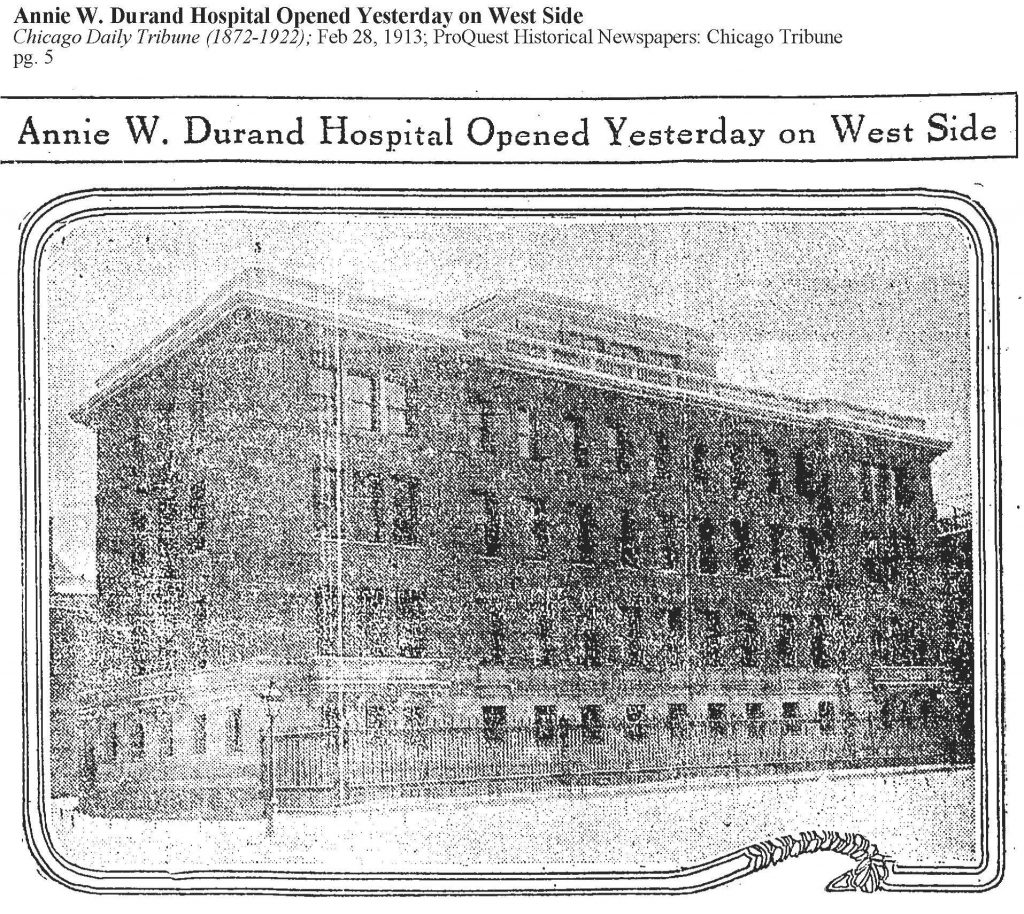
The area was fertile ground for the establishment of major medical institutions and innovative public health dispensaries. Trained medical staff employed experimental therapeutics to respond to the public health crises of water born diseases such as cholera and typhoid, to epidemic diseases such as smallpox and tuberculosis, to childbirth risking the lives of mother and child, to nutritional threats plaguing growing children such as contaminated milk, and to more general threats to child survival such as the factory sweating system.
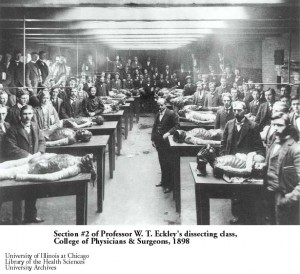
A West Side urban medical district attracted students, patients, and visitors throughout the Midwest. Among the major facilities were Rush Medical College, West Side Hospital, Presbyterian Hospital, Sprague Home for Nurses, Mary Thompson Hospital for Women and Children and Training School for Nurses, College of Physicians and Surgeons (University of Illinois), University of Illinois School of Dentistry, Illinois Training School for Nurses, Chicago Homeopathic College, Cook County Hospital.
As evidenced by the postcard collection, the complex of major institutions in the West Side Medical Center–hospitals, clinics, colleges, training schools, institutes–attracted a significant number of medical staff, students, patients, and visitors from the Midwest. Picture Postcards
Examples of inscriptions appearing on the post cards. On a Rush Medical Hospital Picture Card, a correspondent living in Chicago wrote to a town in Michigan: “Not much to write. All are pretty well only Fred. He is trying to be a Christian and a minister comes in every day to see him.”
On a Presbyterian Hospital, Sprague Home for Nurses picture card, a first-year student nurse wrote home: “Dear Folks. This is where I live now. I was on duty from 8 to 12pm. This afternoon I went for a short walk with 3 girls, two of whom have attended school here three years and know there (sic.) way. I’m hoping to hear from you tomorrow. I like it hear (sic.) fine. Don’t work too hard any of you.” bjb
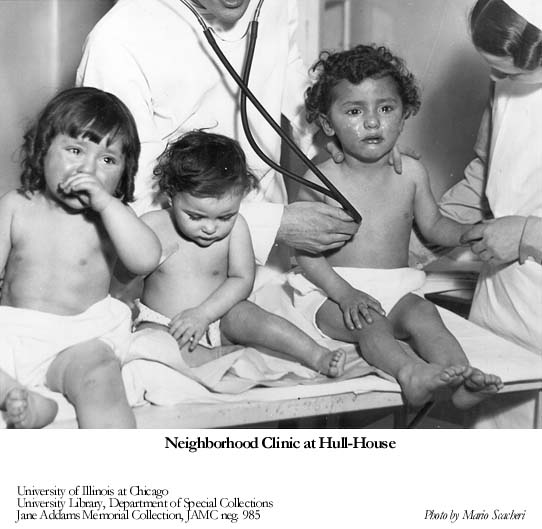
Supported by public and charitable funds, a growing number of neighborhood Dispensaries addressed public health needs by dispensing at no cost medical supplies, pharmaceuticals, treatments, and hygiene education.
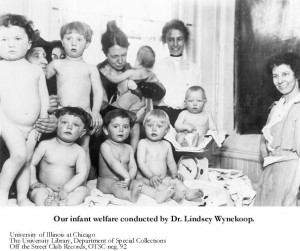
Dr. Joseph B. DeLee, educated in Chicago, founded Chicago Lying In Dispensary on Maxwell Street. He succeeded in moving most childbirths from midwives at home to an equipped hospital theater. Also he was instrumental introducing the first portable infant incubator, improving pediatric techniques and advancing obstetric results. The latter was controversial by advocating for invasive forceps use in childbirth.
In conjunction with Hull-House and its public clinic, Jane Addams founded a Visiting Nurses Association supplying assistance to the working poor in their homes. In 1890 a child in Chicago had only a 50% chance of reaching 5 years of age. By 1900 the odds had improved to 75%, and the rate of infant mortality began dropping. Over time, dental services and eye examinations for school children, including state-of-the-art hygiene practices, made a positive difference in the lives of ordinary people.
In an intriguing “what if” several progressive era reformers proposed national compulsory health insurance covering everyone and embracing all public medical agencies under one government roof. In the Sickness Insurance Law of 1883 Germany had adopted a national social health insurance program. In the 1911 National Insurance Act Britain first adopted a limited primary care program for working-class wage earners. In 1912 Theodore Roosevelt running on the break away “Bull Moose party” platform campaigned for national compulsory health insurance. Jane Addams had seconded Roosevelt’s nomination at the convention.
A strenuous argument for compulsory national insurance–labeled “socialist propaganda and a fanciful scheme” by the private for-profit insurance entrepreneurs–was put forward by Dr. I.M. Rubinow of New York, Chairman of the Health and Public Instruction Committee of the American Medical Association. Rubinow’s accuracy as a statistician was broadly accepted when he observed that roughly 40 percent of wage-earners were sick during the year averaging nine or ten days. Of those some 25 percent were sick over four weeks.
Owing to costs, private health insurance companies failed to cover the medical need with 65 percent of premiums going to company expenses and thirty five percent to beneficiaries. Private insurance company officials blamed badly managed companies for the high numbers whereas their well managed companies held costs down to a mere forty-three percent of premiums!
Nation-wide the opposition prevailed against compulsory health insurance legislation. Government sponsored insurance, the private companies argued, was unproven. A competitive marketplace was the best way forward with “the tendency of the times” to ask the state to do too much for the individual thus taking away personal initiative and responsibility.
One obstacle to legislation was that working people were largely indifferent. Their priority was making up lost wages from unemployment in the present, not be saddled for years with an additional annual insurance expense when the end of life could be relatively sudden and brutish. Consider that in 1910, life expectancy in the U.S. of a “white male” was 48.6 years and white female 52.0 years, a “Negro and Other male” 33.8 years and female 37.5 years. Many years in retirement and illnesses related to longevity were not in the wage-earners ken of experience.
A second obstacle to national legislation was that the American Federation of Labor trade unions led by Samuel Gompers only supported a health benefit secured by the independent unions themselves in packages achieved by each in collective bargaining negotiations.
Finally, The American Medical Association, the establishment professional organization, jealous of its lucrative fee based private doctor-patient relationship remained historically antagonistic to all interference by third-party actors and insurers. (On the AMA see below)
INTRODUCTION
PHOTO GALLERY
- Garbage
- Privies
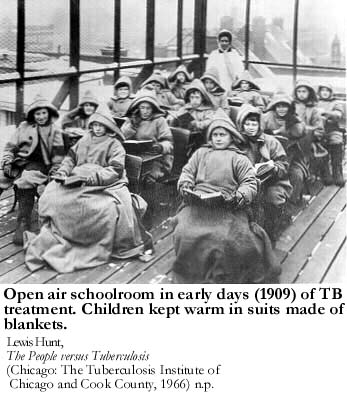
- Tuberculosis
- Dispensaries and Clinics
- Milk
- Medical Training
- Public Health Instruction
- Hospital Postcards
WITCHCRAFT, DEMONS, SICKNESS, and THE HEALING ARTS (1914-1970)
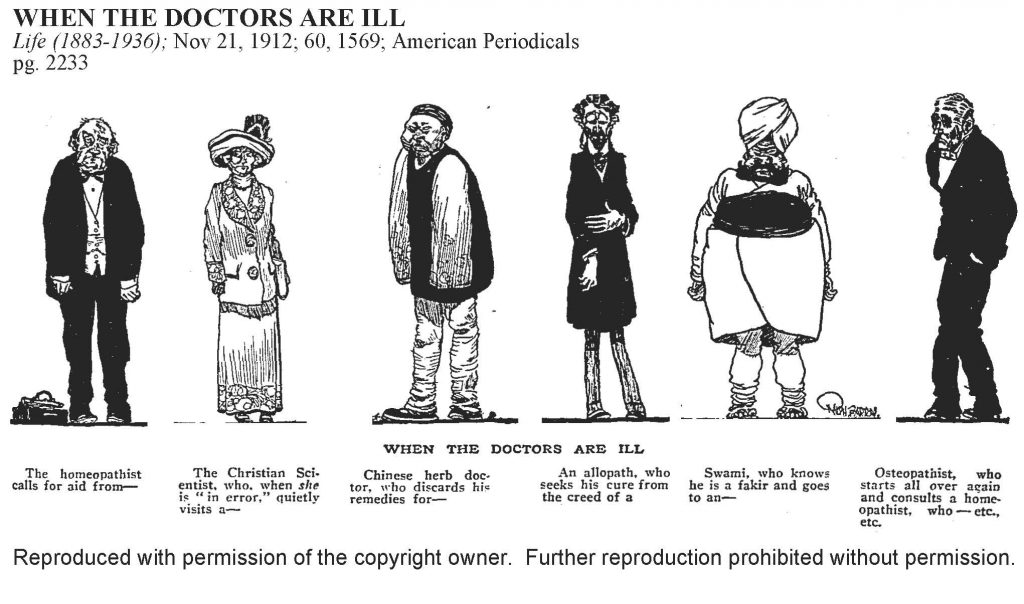
The Dybbuk of Bunker Street, the Devil-Baby at Hull-House, Witchcraft on West Polk: from the perspective of Hull-House residents, the dense neighborhood of “peasants” was overridden by an uncanny alternative universe of animated spirits and miraculous interventions. Entering this alien universe of supernatural phenomena was a steep climb for enlightened and science-minded Hull-House residents.
“We Anglo-Saxons,” Alice Hamilton wrote in a forthright manner, “are dependent on a proper setting for our sense of romance and mystery. To us West Polk street is inconceivable as a background for anything but the drab details of life in a poor neighborhood … with nothing for the imagination to fasten to, no single touch of the weird, the supernatural. But to the Italian these things are as much a part of the real stuff of life as is his job in the street-cleaning gang, his tenement home, the push-carts and garbage wagons on the street.”
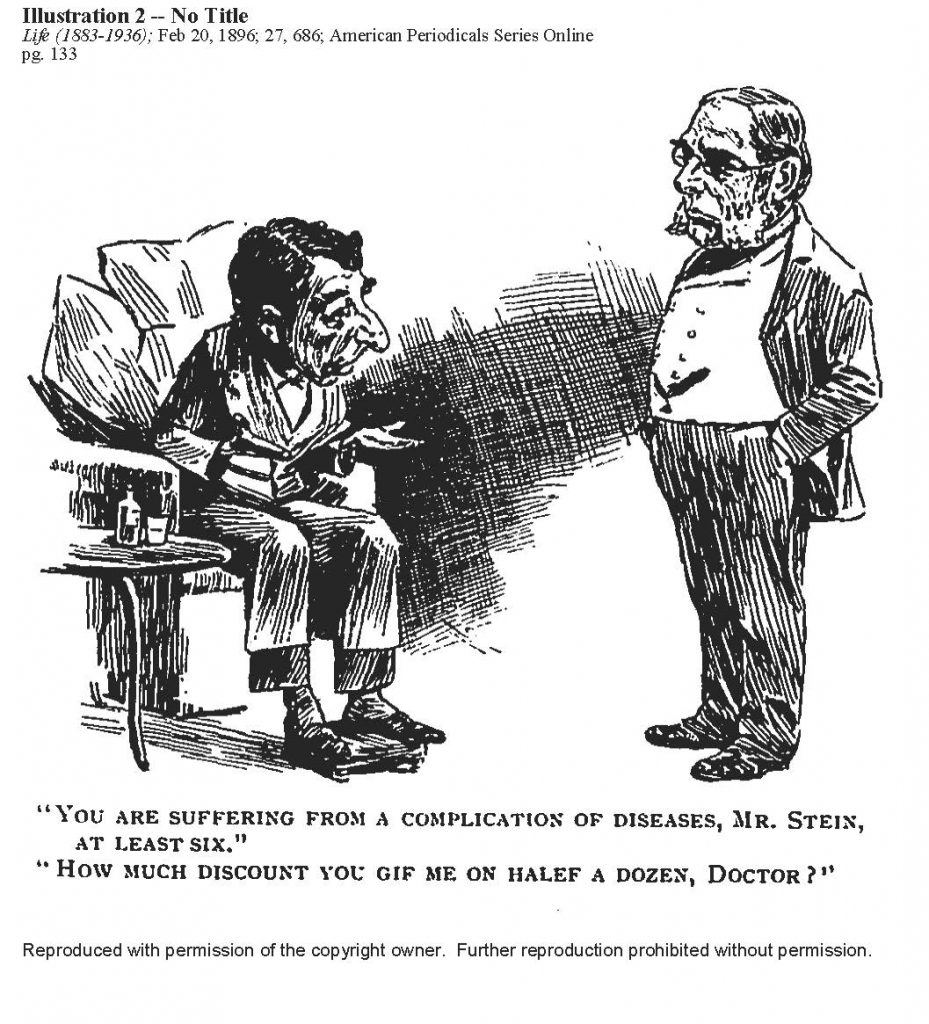
Any form of compulsory health insurance was rare in the early twentieth century. Middle-class Americans paid for health care on a fee-for-service private doctor home visit plan promoted by the established American Medical Association which dominated state licensing and medical review boards. Surgeries, for instance, were often performed in a patient’s home. Morphine remained readily available over the counter until 1914.
Founded in 1847, the professional doctors’ organization lobbied against an expanding group of medical practitioners– “irregulars,” pretenders and quacks all. In the early twentieth century these “incompetents” were found working in low-quality municipal hospitals, under-funded neighborhood clinics, and dispensing quackery within alien and exotic ethnic immigrant enclaves. Street wisdom had it that poor people too sick to work with no one to take care of them at home were sent to municipal hospitals to die. To be hospitalized was a death warrant, allbeit disembodied after an injection of pain-killing “demon rum” and accessible narcotics. bjb
- A Modern Devil Baby by Jane Addams (1914)
- Witchcraft on West Polk Street by Dr. Alice Hamilton (1927)
- The Dybbuk of Bunker Street by Hilda Satt Polacheck (Federal Writers Project 1939)
- An Italian Immigrant in Chicago on American Medicine (1970)
THEODORE B. SACHS, M.D, MAPPING TUBERCULOSIS: WEST SIDE
Born in Russia, Thedore Sachs graduated high school in 1891, and received a degree in law from Odessa University. As a Jewish young man of military age, he was required to report for military duty, and subsequently placed on reserve. After disapproval by authorities of topics he was discussing, he decided like many in his situation that it was time to move to the United States. Preferred to serving as cannon fodder for the Russian military.
Arriving in Chicago he decided to study medicine at the University of Illinois College of Medicine. Recognition of his law degree from a Russian university by the State of Illinois, and a license to practice law were not, in any case, realistic expectations for foreign educated immigrants. Sachs graduated medical school in 1895 and spent two years in internship at Michael Reese Hospital. He then opened a general practice focusing on a widespread affliction in the period, diseases of the lung.
Between 1901 and 1903, Sachs was appointed an instructor in Internal Medicine at the College of Physicians and Surgeons, an Examining Physician at the Maternal Jewish Hospital for Consumptives, and an Attending Physician at Cook County Hospital.
Tuberculosis and related lung diseases were reaching epidemic proportions in polluted sectors on the West Side of Chicago. The poor lived in closed non-ventilated tenement housing where the air was clogged with soot, smoke, and debris from factories, foundries, and piles of uncollected garbage. Infectious diseases favored poverty, overcrowding, and “its unfavorable conditions of life.”
Medical specialists assumed that the Jewish population including recent immigrants experienced lower mortality rates from tuberculosis than other nationalities. They referred to a “race immunity,” in part based on a life-style observing “Kashrut” (dietary laws), habits of cleanliness commanded by “Halachah,” and temperance. Over a period of eighteen months, Sachs proposed to test the assumptions statistically by mapping the mortality and incidence of the disease on the streets of a poor West Side district–the first scientific and statistically-based mapping of its kind in American medicine.
In 1902 upon publication of the results in The Journal of the American Medical Association, recognition and fame came to Sachs. His affiliations as a tuberculosis specialist proliferated, in The Chicago Tuberculosis Institute, The West Side Dispensary, The Chicago Municipal Tuberculosis Sanitarium, the Edward Sanitorium at Naperville. bjb
- Journal of American Medical Association, Tuberculosis in Chicago by Burton J. Bledstein
- Theodore B. Sachs, Tuberculosis in the Jewish District of Chicago (1904)
- A Study of Tuberculosis in Chicago by City Homes Association (1905)
ALICE HAMILTON, M.D, HULL-HOUSE PHYSICIAN, OCCUPATIONAL DISEASES (1903-1919)
Alice Hamilton grew up in Fort Wayne, Indiana in 1869 in a prominent family. After receiving elite eastern schooling, in the 1890s she graduated from medical school, specialized in post-graduate work in Pathology, and began teaching at the Women’s Medical School of Northwestern University. Her interests were focusing on Public Health when she moved into Hull- House as a resident physician and operated a well-baby clinic for neighborhood residents.
At the Hull-House clinic her Anglo-American class prejudices were frontally challenged. Early on she believed “excessive fecundity” of the poor weakened constitutions and their survival rate. The larger the number of children ethnic parents bore, “the more irresponsible and casual and thoughtless” they were. Italian infants in their mother’s arms suckling on salami, and children on the street consuming hot-dogs and ice-cream drove nutrition-minded reformers over the edge of sane response.
In another instance of Anglo bias, Jews had the advantage in overcrowded city tenement life since they had been living in these conditions as outcasts for 2000 years. “By contrast, the Italians, Slavs, Irish, and many German immigrants formerly lived in rural areas. They were peasants, and the life in our cities is for them a sudden and radical change which makes itself felt most disastrously in the health of the first generation born here.” For Hamilton the Hull-House clinic was a learning experience in Public Health.
Her legacy was first made investigating the local neighborhood of the working poor and relating the cause of typhoid epidemics to defective sewers spilling filth on streets lacking sanitation drainage. She also supported the contemporary study of Dr. Theodore Sachs pinpointing the local causes of tuberculosis in the ghetto.
In the industrial workplace, she proceeded to uncover relationships between toxic chemicals–lead, mercury, benzene, radium, aniline dies, carbon and hydrogen gases–and patterns of severe human suffering and mortality for working people. She pioneered in the relatively unknown field of occupational diseases actively rejected by a majority in corporate America. On the epidemiology and toxicology of industrial poisons and the devastating effects, her work and influence were landmarks. bjb
- Alice Hamilton, Resident Physician at Hull-House by Ellen Skerrett
- An Inquiry into the Causes of the Recent Epidemic of Typhoid Fever in Chicago (1903)
- The Social Settlement and Public Health (1907)
- Industrial Diseases (1908)
- The Fly as a Carrier of Typhoid (1909)
- Industrial Poisons Used in the Lead Industry (1915)
- Women in the Lead Industries (1919)
MAX THOREK: NEIGHBORHOOD ETHNIC DOCTOR
Max Thorek was born in a mountain region of Hungary to a Jewish family. His father was a rural doctor and mother a midwife. Among his earliest memories were religious hatreds between the Calvinist minority and the Catholic majority and class differences cemented by an entrenched political feudalism
Thorek was attending a Gymnasium in Budapest when a pogrom abetted by the local police targeted Jews. Savage barbarisms were committed against the “bastard Christ Killers,” and in a night of terror, his brother was among those killed. Hungary now became “forever an alien homeland,” and with the sponsorship of a rich uncle in America, the family chose to sail steerage from the port of Bremen with a destination, Chicago Illinois.
Living on the West Side with his mother practicing as a midwife, the family struggled to subsist. Thorek talked an administrator at the University of Chicago into a fellowship as a snare drummer in the University band, an instrument he had no knowledge of. A summer’s practice made his proficient. He entered Rush Medical College affiliated with the University. Over the next years he specialized in obstetrics becoming an M.D., interned at Marcy Home on Maxwell Street, started his own neighborhood practice, became an Associate in gynecology at the West Side Hospital and a consulting staff member at Cook County Hospital.
With improved English and a pleasing manner, Thorek’s practice became large and profitable, and he realized his wish to become a general surgeon and found his own hospital, at first in rented quarters on the West Side.
At once, ambitious, confident, and congenial, Thorek flourished in an exemplary career never losing sight of his prmary identity as an ethnic neighborhood doctor. bjb
Max Thorek, A Surgeon’s World: An Autobiography (1943)
- Chapter 1. First Memories, pp. 13-21
- Chapter 2. Struck By Lightning, pp. 22-29
- Chapter 3. Student in Budapest, pp. 30-38
- Chapter 4. Lost Homeland, pp. 39-43
- Chapter 5. My Uncle Bernard, pp. 44-49
- Chapter 6. Fiddle and Drum, pp. 51-60
- Chapter 7. Discipline of Aesculapius, pp. 61-75
- Chapter 8. Mystery of Birth, pp. 76-89
- Chapter 9. Practicing Physician, pp. 90-106
- Chapter 10. Up the Ladder, pp. 110-117
- Chapter 12. Full Speed Ahead, pp. 134-139
- Chapter 14. Thoughts on Turning Forty, pp. 153-156